Intro
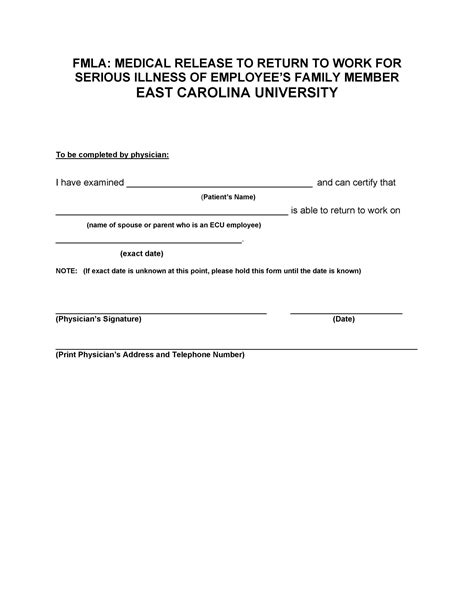
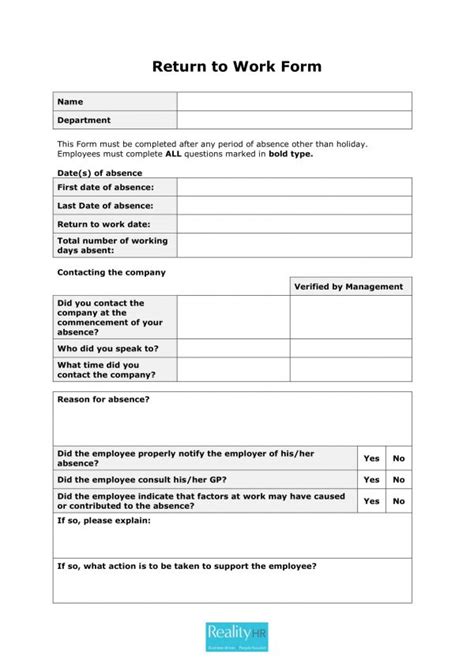
Get a Return To Work Doctor Note Template to ease employee transitions. Includes medical clearance, work restrictions, and fitness for duty assessments, streamlining HR processes and ensuring a smooth return to work after illness or injury.
The process of returning to work after a period of illness or injury can be complex, involving various stakeholders including employers, healthcare providers, and the employees themselves. A crucial document in this process is the return to work doctor note, also known as a fitness for duty note. This document serves as formal communication from a healthcare provider to an employer, confirming that an employee is fit to resume their job duties following a period of absence due to health reasons.
Return to work doctor notes are essential for several reasons. Firstly, they provide legal protection for both the employee and the employer. For the employee, it ensures that they are not forced back to work before they are medically ready, which could exacerbate their condition. For the employer, it provides documentation that the employee has been cleared by a medical professional, reducing the risk of workplace accidents or further health complications.
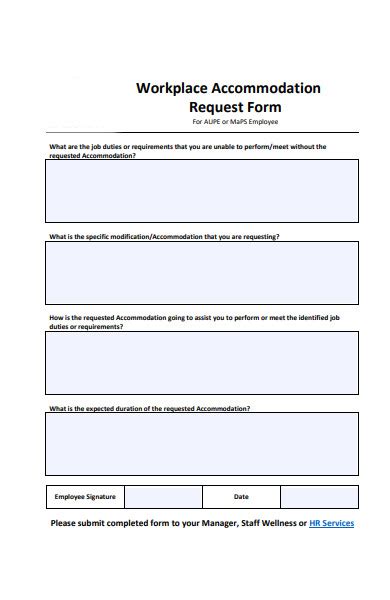
Secondly, these notes facilitate a smooth transition back to work. They can include recommendations for temporary modifications to the employee's job duties or work environment to ensure a safe and successful return. This might involve reducing working hours, altering tasks to avoid exacerbating the condition, or providing ergonomic adjustments to the workspace.
However, the process of obtaining and utilizing return to work doctor notes can be cumbersome. Employees might face challenges in scheduling appointments with their healthcare providers, and there could be delays in receiving the necessary documentation. Employers, on the other hand, must balance the need to accommodate returning employees with the operational demands of their business.
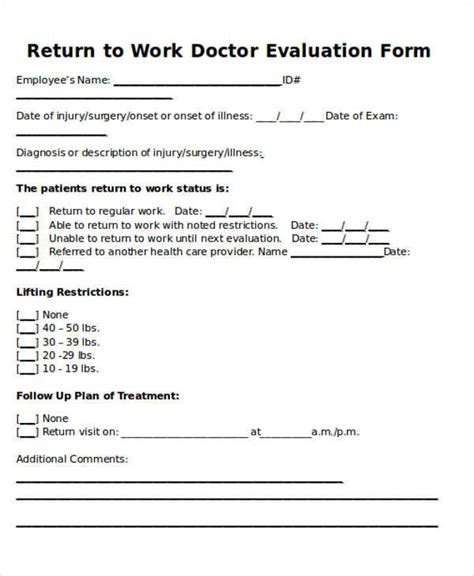
Given these considerations, it's beneficial to have a template for return to work doctor notes that can streamline the process while ensuring all necessary information is included. A typical template should cover the following elements:
- Employee Information: Full name, date of birth, and job title.
- Healthcare Provider Information: Name, title, contact information, and medical license number.
- Dates of Absence and Anticipated Return: Clearly stating the period the employee was absent and the date they are cleared to return to work.
- Medical Condition: A brief description of the condition that led to the absence, without revealing sensitive medical information.
- Fitness for Duty: A statement confirming the employee is fit to return to work, including any limitations or restrictions.
- Recommended Accommodations: Details on any temporary adjustments needed to facilitate the employee's return to work safely.
- Follow-Up Care: Instructions for any ongoing medical care or follow-up appointments that may impact work schedules.
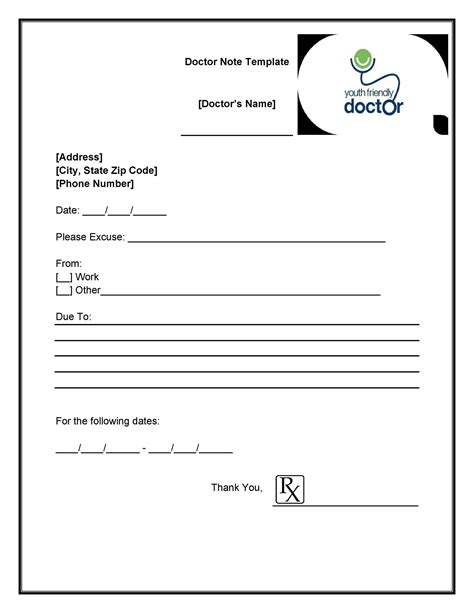
Here is a basic template that can be adapted based on specific needs and circumstances:
[Healthcare Provider's Letterhead or Medical Facility's Letterhead]
[Date]
[Employer's Name]
[Employer's Title]
[Company Name]
[Company Address]
Dear [Employer's Name],
Re: [Employee's Name] - Return to Work Clearance
I am writing to confirm that [Employee's Name], who has been under my care for [briefly mention the condition], is now cleared to return to work. The details of their employment and medical clearance are as follows:
- Employee Name: [Employee's Full Name]
- Date of Birth: [Employee's Date of Birth]
- Job Title: [Employee's Job Title]
- Dates of Absence: [Start Date] to [End Date]
- Anticipated Return to Work Date: [Date]
After a thorough evaluation and completion of the necessary treatment, I am pleased to state that [Employee's Name] has made sufficient progress to resume their job duties. However, to ensure a safe and successful return to work, I recommend the following accommodations:
[List any recommended accommodations, such as reduced hours, avoidance of heavy lifting, etc.]
Please note that these recommendations are temporary and are intended to support [Employee's Name] during their transition back to full duty. I anticipate that these accommodations will be necessary for [specify timeframe] and will reassess as necessary.
If you have any questions or concerns regarding this clearance or the recommended accommodations, please do not hesitate to contact me at [Your Contact Information].
Thank you for your understanding and support in [Employee's Name]'s return to work.
Sincerely,
[Your Name]
[Your Medical Title]
[Medical License Number]
[Contact Information]

Understanding the Components of a Return to Work Doctor Note
A return to work doctor note is a multifaceted document that requires careful consideration of various components to ensure it serves its purpose effectively. Each section of the note, from the employee's and healthcare provider's information to the details of the medical condition and recommended accommodations, plays a critical role in facilitating a successful return to work.

Employee and Healthcare Provider Information
The note should clearly identify both the employee and the healthcare provider. This includes full names, professional titles, and contact information. The healthcare provider's medical license number may also be included for verification purposes.
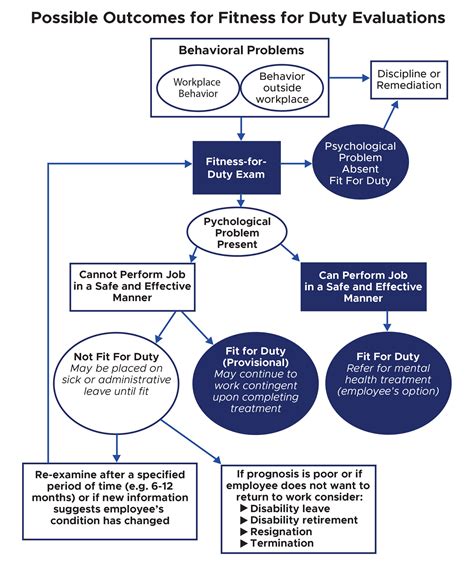
The Role of Return to Work Doctor Notes in Workplace Safety
Return to work doctor notes are not just about confirming an employee's fitness to resume their duties; they also play a significant role in maintaining workplace safety. By ensuring that employees are medically cleared to return to work and specifying any necessary accommodations, these notes help prevent workplace accidents and reduce the risk of further injury or illness.

Preventing Workplace Accidents
One of the primary ways return to work doctor notes contribute to workplace safety is by preventing accidents. When an employee returns to work too soon or without proper clearance, they may not be fully capable of performing their duties safely. This can lead to accidents, not only harming the employee but also potentially affecting their colleagues.
Best Practices for Implementing Return to Work Programs
Implementing an effective return to work program involves several best practices, from maintaining open communication with employees to ensuring that all return to work doctor notes are thoroughly reviewed and acted upon. Employers should also be proactive in offering support and accommodations to facilitate a smooth transition back to work.

Maintaining Open Communication
Open and honest communication is key to a successful return to work program. Employers should keep lines of communication open with employees throughout their absence and return. This includes discussing the employee's progress, any challenges they might face upon returning, and how the employer can support them.
Challenges and Solutions in the Return to Work Process
Despite the importance of return to work doctor notes and programs, several challenges can arise. These might include delays in receiving medical clearance, difficulties in implementing recommended accommodations, and ensuring that the return to work process is fair and consistent for all employees.
Delays in Receiving Medical Clearance
One common challenge is the delay in receiving the return to work doctor note. This can be due to scheduling issues with healthcare providers or the time it takes to complete the necessary treatment and evaluation. Employers and employees can mitigate this by planning ahead, scheduling follow-up appointments in advance, and maintaining regular communication with healthcare providers.
Return to Work Doctor Note Image Gallery



What is a return to work doctor note?
+A return to work doctor note is a document from a healthcare provider that confirms an employee is fit to return to work after a period of absence due to illness or injury.
Why are return to work doctor notes important?
+These notes are crucial for ensuring that employees are medically cleared to resume their duties, preventing workplace accidents, and facilitating a smooth transition back to work.
What information should a return to work doctor note include?
+A return to work doctor note should include the employee's and healthcare provider's information, dates of absence and anticipated return, a brief description of the medical condition, confirmation of fitness for duty, and any recommended accommodations.
How can employers support employees returning to work?
+Employers can support returning employees by maintaining open communication, offering necessary accommodations, and ensuring a safe and welcoming work environment.
What are some common challenges in the return to work process?
+Common challenges include delays in receiving medical clearance, difficulties in implementing recommended accommodations, and ensuring fairness and consistency in the return to work process for all employees.
As we conclude our discussion on return to work doctor notes and their significance in facilitating a safe and successful return to work, it's essential to remember that these documents are just one part of a broader strategy to support employee health and well-being. By understanding the importance of return to work doctor notes, implementing effective return to work programs, and addressing the challenges that arise, employers can create a positive and productive work environment that benefits both the organization and its employees. We invite you to share your thoughts and experiences with return to work processes, and we look forward to continuing this conversation on how to best support employees as they return to work after a period of absence.
