Intro
Improve pharmacy operations with 5 key policy tips, enhancing patient care, medication management, and regulatory compliance, while optimizing pharmacy services and healthcare outcomes.
The importance of a well-structured pharmacy policy cannot be overstated. A clear and comprehensive policy is essential for ensuring the safe and effective use of medications, protecting patients from potential harm, and promoting optimal health outcomes. In today's fast-paced healthcare environment, pharmacies play a critical role in providing high-quality patient care, and a well-defined policy is vital for guiding their operations. By establishing a robust pharmacy policy, healthcare organizations can minimize errors, reduce risks, and improve patient satisfaction.
Effective pharmacy policies are designed to promote safe and responsible medication use, prevent adverse reactions, and optimize therapeutic outcomes. A well-crafted policy should address key aspects of pharmacy operations, including medication ordering, dispensing, and administration, as well as patient counseling and education. By establishing clear guidelines and protocols, pharmacies can ensure that patients receive the right medication, in the right dose, at the right time, and with proper instructions for use. Moreover, a comprehensive pharmacy policy can help healthcare organizations stay compliant with regulatory requirements, reduce liability risks, and maintain accreditation standards.
The development and implementation of a pharmacy policy require careful planning, collaboration, and communication among healthcare stakeholders, including pharmacists, physicians, nurses, and other healthcare professionals. A well-structured policy should be based on evidence-based practices, reflect current clinical guidelines, and incorporate feedback from patients, families, and caregivers. By engaging stakeholders in the policy development process, healthcare organizations can ensure that their pharmacy policy is patient-centered, effective, and responsive to emerging healthcare needs. In this article, we will discuss five essential pharmacy policy tips that can help healthcare organizations establish a robust and effective policy framework.
Tip 1: Establish Clear Medication Use Policies
To establish clear medication use policies, healthcare organizations should engage stakeholders in the policy development process, including pharmacists, physicians, nurses, and other healthcare professionals. The policy should be based on evidence-based practices, reflect current clinical guidelines, and incorporate feedback from patients, families, and caregivers. The policy should also be regularly reviewed and updated to ensure that it remains relevant, effective, and responsive to emerging healthcare needs.
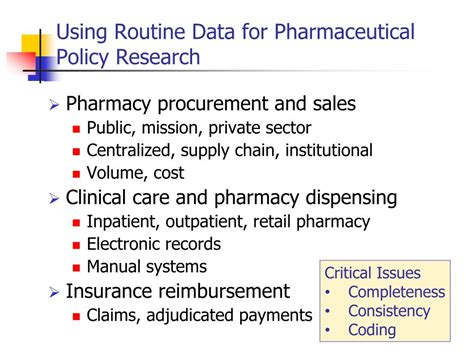
Tip 2: Develop a Comprehensive Pharmacy Quality Assurance Program

To develop a comprehensive pharmacy quality assurance program, healthcare organizations should establish a quality assurance committee that includes representatives from pharmacy, medicine, nursing, and other healthcare disciplines. The committee should be responsible for developing and implementing quality assurance policies and procedures, as well as monitoring and evaluating pharmacy operations. The program should also include mechanisms for reporting and addressing quality issues, such as medication errors and adverse reactions.
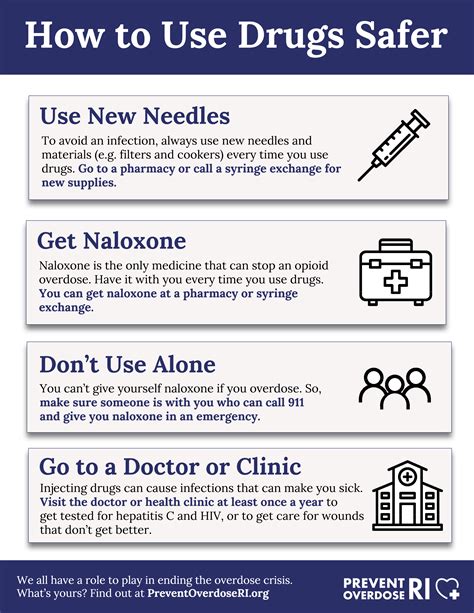
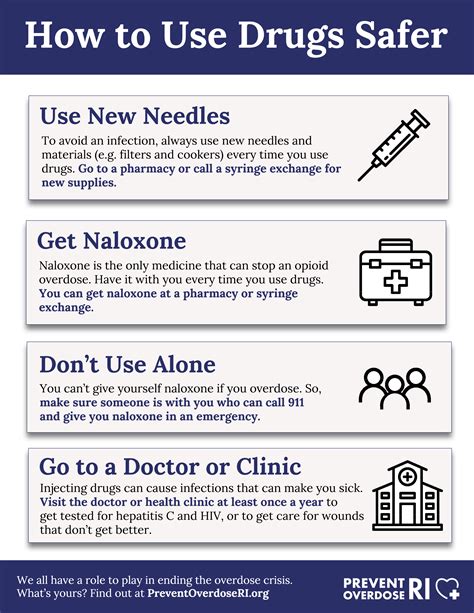
Tip 3: Implement Robust Patient Counseling and Education Policies
To implement robust patient counseling and education policies, healthcare organizations should establish a patient counseling and education program that includes trained pharmacists and other healthcare professionals. The program should be designed to meet the unique needs of patients, including those with limited health literacy, language barriers, and cultural differences. The policy should also include mechanisms for evaluating patient outcomes and assessing the effectiveness of patient counseling and education services.
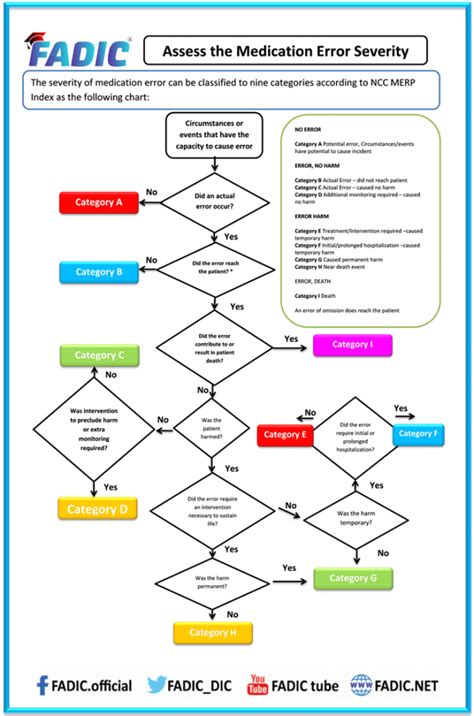
Tip 4: Establish Clear Policies for Medication Error Reporting and Management
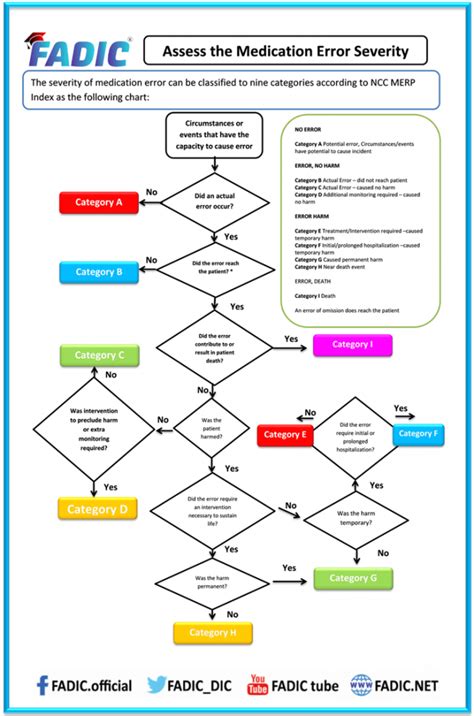
To establish clear policies for medication error reporting and management, healthcare organizations should establish a medication error reporting system that includes a clear and confidential reporting process, as well as a thorough investigation and analysis of reported errors. The policy should also include protocols for addressing and preventing future errors, such as changes to medication ordering, dispensing, and administration processes. The policy should be regularly reviewed and updated to ensure that it remains effective and responsive to emerging healthcare needs.
Tip 5: Develop a Comprehensive Pharmacy Staff Training and Development Program

To develop a comprehensive pharmacy staff training and development program, healthcare organizations should establish a training and development committee that includes representatives from pharmacy, medicine, nursing, and other healthcare disciplines. The committee should be responsible for developing and implementing training and development policies and procedures, as well as evaluating the effectiveness of training and development programs. The program should include mechanisms for assessing staff knowledge and skills, providing feedback and coaching, and evaluating the impact of training and development on patient outcomes.
Gallery of Pharmacy Policy Images
Pharmacy Policy Image Gallery






What is the purpose of a pharmacy policy?
+The purpose of a pharmacy policy is to ensure the safe and effective use of medications, protect patients from potential harm, and promote optimal health outcomes.
How can healthcare organizations develop a comprehensive pharmacy policy?
+Healthcare organizations can develop a comprehensive pharmacy policy by engaging stakeholders in the policy development process, including pharmacists, physicians, nurses, and other healthcare professionals. The policy should be based on evidence-based practices, reflect current clinical guidelines, and incorporate feedback from patients, families, and caregivers.
What are the key components of a pharmacy policy?
+The key components of a pharmacy policy include medication use policies, pharmacy quality assurance programs, patient counseling and education policies, medication error reporting and management policies, and pharmacy staff training and development programs.
In
